Diabetes Can Affect Sight
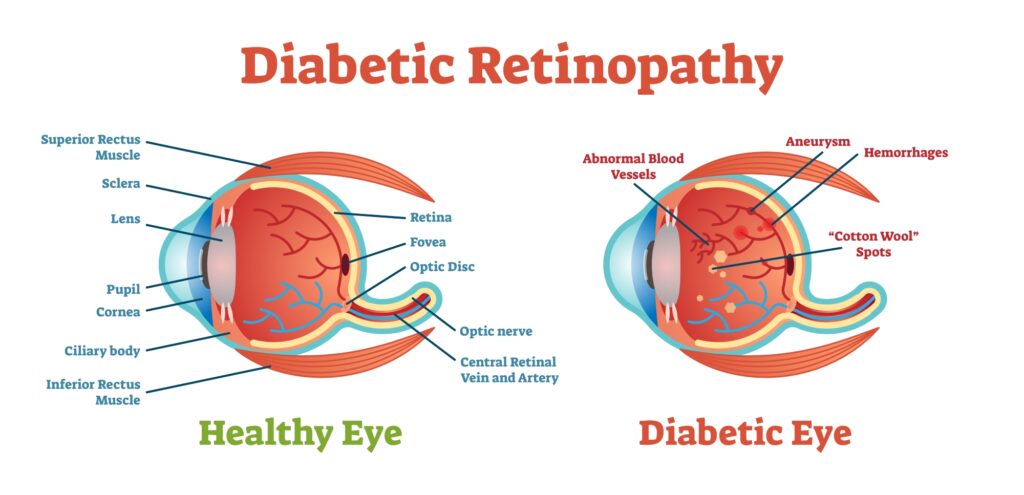
If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and sends images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Types Of Diabetic Retinopathy
There are two types of diabetic retinopathy: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.
PDR is present when abnormal new vessels begin growing on the surface of the retina or optic nerve. The main cause of PDR is widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where original vessels closed.
Unfortunately, the new abnormal blood vessels do not resupply the retina with normal blood flow. The new vessels are often accompanied by scar tissue that may cause wrinkling or detachment of the retina.
How Is Diabetic Retinopathy Diagnosed?
A medical eye examination is the only way to find changes inside your eye. An eyecare professional can often diagnose and treat serious retinopathy before you are aware of any vision problems. The eyecare professional dilates your pupil and looks inside of the eye with an ophthalmoscope.
If your doctor finds diabetic retinopathy, he or she may order color photographs of the retina or a special test called fluorescein angiography to find out if you need treatment. In this test a dye is injected in your arm and photos of your eye are taken to detect where fluid is leaking.
How Is Diabetic Retinopathy Treated?
The best treatment is to prevent the development of retinopathy as much as possible. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss from diabetic retinopathy. If high blood pressure and kidney problems are present, they need to be treated.
- Laser surgery: Laser surgery is often recommended for people with macular edema, PDR and neovascular glaucoma.
- Intravitreal injections: An in office procedure where medication is injected directly into the vitreous cavity of the eye to decrease macular edema, thereby increasing the visual acuity. The effects of the medication last up to three months and repeat injections are needed in order to maintain the beneficial effects.
- Vitrectomy: In advanced PDR, the ophthalmologist may recommend a vitrectomy. During this microsurgical procedure, which is performed in the operating room, the blood-filled vitreous is removed and replaced with a clear solution. The ophthalmologist may wait for several months or up to a year to see if the blood clears on its own before performing a vitrectomy.
Vision Loss Is Largely Preventable
If you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against loss of vision.
You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar and visiting your ophthalmologist regular.